Acute Airway Obstruction After Percutaneous Tracheostomyby J. Heath Brasher, DO and Kevin W. Hatton, MD, FCCM
Fall 2018 NewsletterBackground: Case Report: Because of the patient’s clinical deterioration and x-ray results, emergent bronchoscopy was performed to restore left lung ventilation and assess possible causes of lung collapse. The bronchoscope was passed through the newly-placed tracheostomy into the left mainstem bronchus, which, on initial evaluation, appeared to be filled with clear fluid that could not be suctioned from the bronchus. (Figure 2) After additional inspection, this clear fluid appearance was due to a clear plastic foreign body (FB) in the left mainstem bronchus, completely obstructing the left lung. (Figure 3) The FB was then removed from the airway by bronchoscopic suctioning. The patient’s post-bronchoscopy chest x-ray showed resolution of her left lung collapse. (Figure 4) Discussion We believe that the clear plastic FB was mostly likely caused by a tear in the endotracheal tube (ETT) cuff at the time of the procedure, primarily because the ETT was not pulled back far enough before the introducer needle was advanced into the trachea. In this situation, the introducer needle most likely perforated the endotracheal tube balloon during percutaneous entry. Air was aspirated by the surgeon from the cuff, although, at the time, he believed he was withdrawing air from the trachea. The surgeon did not recognize the error and advanced the guidewire through the introducer needle, into the airway, likely causing a second hole in the ETT cuff. When the dilator was then advanced over the guidewire, the torn ETT cuff was advanced into the airway where it became lodged in the left mainstem bronchus. In discussion with the surgery team, they reported use of bronchoscopy prior to the procedure and after the tracheostomy was placed but did not utilize bronchoscopy in real time to monitor the procedure from inside the tracheostomy as it was being performed. This complication may have been avoided if real time bronchoscopy was used to visualize percutaneous placement of the introducer needle, guidewire, dilator and tracheostomy. Fortunately, emergent bronchoscopy was able to remove this clear, plastic foreign body. Rigid bronchoscopy or other, more advanced, therapies may have been necessary to restore bilateral ventilation if bronchoscopy had failed. Complications of tracheostomies have been reported to occur in approximately 15% of patients.(1,2) The majority of which occur greater than one week after procedure. Complications are generally divided into short and long term. Short term complications include hemorrhage, infection, pneumothorax, tracheostomy tube obstruction, and accidental decannulation. Long term complications include tracheomalacia, trachea-innominate artery fistula, tracheoesophageal fistula, pneumonia, aspiration, granuloma, airway stenosis, and decannulation failure.(1-4) Airway obstruction accounts for 18.5% of these complications, most commonly attributed to mucus plugging.(3-4) In summary, we report an uncommon cause of post-procedure hypoxemia after seemingly-uncomplicated percutaneous tracheostomy caused by inadvertent and unrecognized ETT cuff tear. Critical care anesthesiologists should be cognizant of this possibility in unexplained hypoxemia, especially with lobar consolidation on CXR, following percutaneous tracheostomy. References
Figures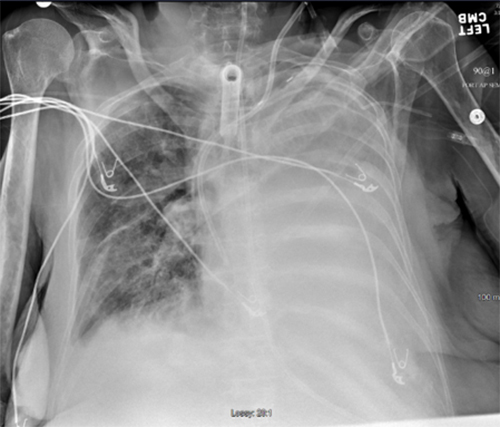 Figure 1: Chest x-ray taken during desaturation event. 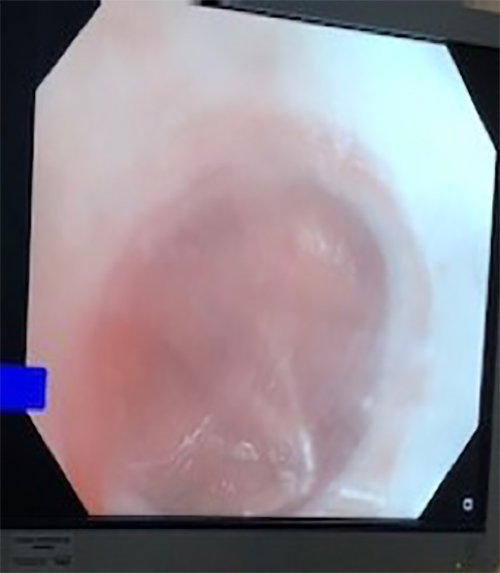 Figure 2: Bronchoscopic view of clear fluid  Figure 3: Bronchoscopic view of clear plastic along lower right border of image 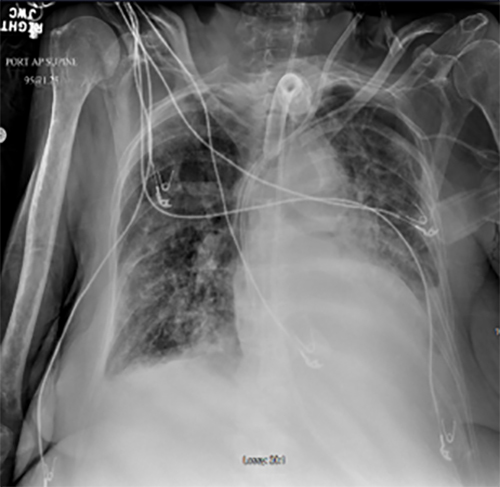 Figure 4: Chest x-ray after removal of clear plastic foreign body and post-obstruction secretions Authors |